What Foods Trigger IBS Attacks?
What foods trigger IBS attacks?
How do you prevent IBS flare-ups?
Best IBS diet?
Best IBS supplements?
We will discuss IBS symptoms, causes, best IBS diet, the 5R approach and alternative recommendations including supplements and lifestyle.
Let’s get started!
This information is for educational purposes only. As with any medical advice, always check with your doctor or healthcare professional for personal and age-appropriate recommendations.
Table of Contents
What is IBS?
IBS or irritable bowel syndrome is a digestive disorder that affects about 10-20% of the population (1, 2). The actual cause is unclear however, according to the ROME criteria, it can present in 3 different ways (3).
The 3 types of IBS are (4, 5).
IBS-D (diarrhea)
- characterized by multiple loose stools.
IBS-C (constipation)
- a type of IBS which often shows up as abdominal pain and bloating with constipation having less than 3 stools per week.
IBS-M (mixed)
- alternating between both diarrhea and constipation.
Bristol Stool Chart PDF
A free Bristol Stool Chart can be found here Bristol Stool Chart.
It can be helpful in reviewing stool consistency. See below for a definition.
- Type 1: Separate, hard lumps
- Type 2: Sausage like but lumpy
- Type 3: Like a sausage but with cracks in the surface
- Type 4: A soft sausage or snake that is smooth
- Type 5: Soft blobs with clear cut edges
- Type 6: Mushy stools with ragged edges
- Type 7: Liquid, watery, no solid pieces
Types 1 and 2 are constipated, Types 3-5 are normal and types 6 and 7 are loose.
What are Symptoms of IBS?
- Diarrhea
- Constipation
- Abdominal pain
- Bloating
- Gas
- Weight loss
- Nausea
What Contributes to IBS Symptoms?
The cause of IBS is unclear however, inflammation may play a role and there may be several contributing causes (6).
A recent article in 2020 discusses some of the causes of functional gastrointestinal disorders including a gut-brain connection, inflammation, gut pathobiome, and gastrointestinal function (7).
Neuroinflammation: The Gut-Brain Connection
Anxiety, stress, depression, and adverse childhood experiences (ACEs) may increase the risk of IBS. The gut-brain connection plays a role in IBS (8, 9).
There is increased interest in the communication between the nervous system and the immune system and its contribution to IBS symptoms. Immune mediators may be released from mast cells which may lead to increase pain with IBS (10).
Imbalance of the Microbiome
Dysbiosis (an imbalance in gut bacteria) can contribute to IBS (11). An imbalance of gut bacteria can cause the immune system in the gut to activate causing inflammation.
Post Infectious Gastroenteritis
A food poisoning event can increase the risk of IBS (often called post-infectious IBS). Systemic inflammation and altered microbiome diversity can contribute to symptoms. (12).
There has been recent research on the relationship of food triggers and gut-brain disorders related to various factors including digestion, visceral hypersensitivity, immune response, and the gut-brain connection (13).
Intestinal Barrier Dysfunction
A review of 66 studies showed that intestinal barrier dysfunction was present in a large portion of patients with IBS. Loss of barrier function contributed to abdominal pain and changes in bowel function (14).
Diet and stress may contribute to changes in your gut microbes and changes in gut health.
What is Post-Infectious IBS?
Post-infectious IBS means IBS symptoms that occur after an infection (either bacterial or parasitic).
Symptoms of IBS such as diarrhea and abdominal pain may occur after a case of gastroenteritis. Do you know anyone who has continued gut challenges after a case of food poisoning? Symptoms may persist for a long time and be like symptoms of IBS-D (15).
Use of antibiotics exerts a negative effect on gut health causing dysbiosis which is a major factor in post-infectious IBS (16).
5R Approach for Gut Healing
The 5R approach is a 5 step process to heal the gut.
The steps are:
- Remove- remove the irritant which may be food, a parasite, stress
- Replace- replace enzymes, hydrochloric or bile acids and nutrients
- Reinoculate- increase beneficial bacteria adding pre and probiotics
- Repair- add gut healing nutrients
- Rebalance- rebalance with lifestyle changes
A functional stool test analyzes gut health which can be a helpful tool guiding the 5R approach.
Following this protocol can improve IBS symptoms.
What Foods Trigger IBS Attacks?
There are many foods which may trigger IBS symptoms. Some of the more common foods include processed foods, gluten, dairy, and high FODMAP (fermentable oligo-, di-, and monosaccharides and polyols) foods (17, 18).
An anti-inflammatory diet may reduce IBS symptoms.
Best IBS Diet: Anti-Inflammatory Diet for IBS
FODMAP
A low FODMAP is a very common diet recommended for IBS (19, 20). Studies show symptom reduction is seen in about 50-80% of patients who follow a low FODMAP diet however, it also can lead to changes in the gut microbiota.
A low FODMAP diet is followed short term (2-6 weeks) then, a challenge phase of food reintroduction with FODMAPS is recommended.
Low FODMAP stands for:
F- Fermentable (fermentable foods that move through the gut and produce gas)
O- Oligosaccharides (Fructans and GOS found in wheat, onion, garlic, beans)
D- Disaccharides (Lactose found in dairy)
M- Monosaccharides (Fructose in high fructose corn syrup, honey, and fruits)
And
Polyols (Sugar alcohols like Sorbitol and mannitol often found in artificial sweeteners)

Mediator Release Test (MRT) and the LEAP Protocol
MRT is a blood test that measures your sensitivity to 170 food and food chemicals. It measures the amount of mediators released from your white blood cells when exposed to food antigens and food chemicals.
From the MRT results, a Registered Dietitian or healthcare practitioner creates a LEAP protocol based on your results, medical history, and lifestyle. We typically see significant symptom reduction in the first 2 weeks.
The LEAP protocol allows for a more personalized nutrition approach to healing. There is ongoing research on MRT, and the LEAP protocol being conducted (21).

Best Supplements for IBS
Many supplements may reduce symptoms of IBS. The supplementation recommendation depends on symptoms present and results of gut testing.
Vitamin D for Leaky Gut
Optimizing vitamin D contributes to improved immune function and bone health. Low vitamin D is common in IBS and optimizing levels may improve IBS symptoms (22, 23). Vitamin D deficiency may be associated with leaky gut (24).
Magnesium for IBS-C
Magnesium is involved in over 600 pathways in the body (25).
Certain forms of magnesium loosen stools and may reduce constipation in IBS-C (26).
Magnesium citrate is one form that helps with constipation and it is readily available in capsules, liquid, and powder forms.
Partially Hydrolyzed Guar Gum (PHGG) Fiber for IBS
There are 2 types of fiber, soluble and insoluble. Soluble fiber appears to reduce IBS symptoms (27).
PHGG is effective in the treatment of IBS-C as shown in recent studies and it also has prebiotic effects (28, 29).
Psyllium for Constipation
What about psyllium? Psyllium is also a soluble fiber that acts as a gel thickening up loose stools and reducing constipation.
All fiber supplementation should be started slowly and increased in small amounts as tolerated (30).
Be cautious of the type of fiber used as not all fibers improve IBS symptoms.
Peppermint for IBS
Enteric coated peppermint may help by soothing the smooth muscle and preventing spasms (may be contraindicated in reflux).
Nine studies were reviewed, and peppermint oil was found to be a safe short term treatment for IBS (31). Another meta-analysis of 12 studies with peppermint was shown to be effective for abdominal pain and other symptoms of IBS (32).
Colostrum for Gut Health
Colostrum is a nutrient rich supplement with healing properties for the gut.
A 2022 study reviewed various nutraceuticals including colostrum and showed restoration of gut function (33).
As with other supplements, start slowly when taking colostrum.
Saccharomyces Boulardii for IBS
S. Boulardii is a yeast probiotic beneficial for digestive disorders (34). This probiotic has been prescribed for antibiotic associated diarrhea, C difficile, and bowel disease.
A 2021 review of studies showed reduction of abdominal pain with S. Boulardii (35).
Zinc Carnosine for Gut Healing
Zinc deficiency is common among people with IBS-D (36). Zinc carnosine promotes healthy gut tissue and has been shown to heal the gut mucosa (37, 38).
There are many other supplements which may be recommended after stool or micronutrient testing depending on test results and symptoms present.
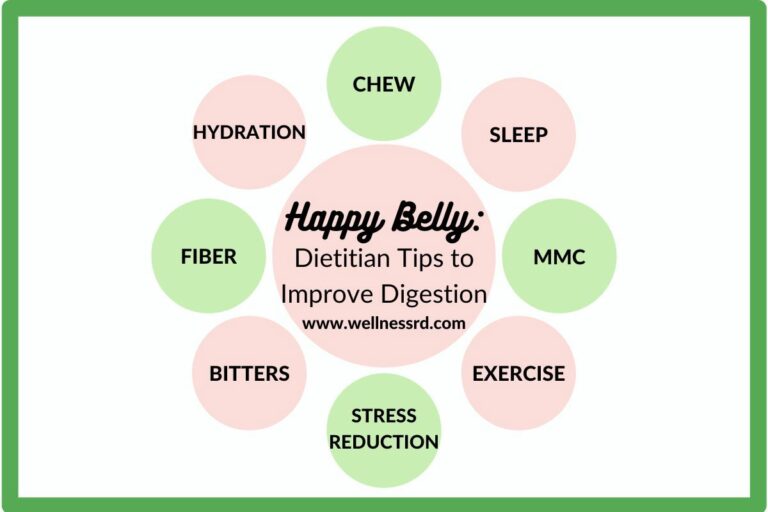
Lifestyle Modification for IBS
Engaging in a healthy lifestyle may improve IBS symptoms.

Mindfulness
Being mindful is the state of being in the moment with our thoughts, feelings, body, and environment.
Mindful Based Stress Reduction (MBSR) is one program that improves GI symptoms (39). There are many other programs as well as cognitive behavioral therapy that may be beneficial in improving gut-brain communication (40, 41).
Sleep
Poor sleep is common in IBS and correlates with IBS pain (42).
A study of adolescents with IBS results showed 53% had a sleep disorder (43). The prevalence of sleep disorders is high among individuals with IBS and more research is needed to understand the relationship of sleep and IBS (44).
There are many strategies to improve sleep including mindfulness, limiting screen time before bed, sleeping in a cool room, and supplements such as magnesium, theanine, and melatonin.
Visceral Manipulation
Studies have shown visceral manipulation may be beneficial in symptom reduction of IBS as patients may present with visceral hypersensitivity (45, 46, 47).
Final Thoughts
In conclusion, IBS or irritable bowel syndrome is a digestive disorder that affects about 10-20% of the population and presents with diarrhea, constipation, or mixed.
A Bristol Stool Chart reviews stool consistency.
First, the 5R approach may help guide the steps for healing the gut. A stool test can be an important tool.
Also, an elimination diet can be followed for symptom reduction.
A low FODMAP diet may reduce symptoms in some individuals however, it should only be followed short term (2-6 weeks) then, FODMAP foods are reintroduced.
MRT is a food sensitivity blood test which allows for a more personalized nutrition approach with the LEAP protocol.
Next, some supplements which may be beneficial for IBS include vitamin D, magnesium, PHGG, psyllium, peppermint, colostrum, S. Boulardii and zinc carnosine.
Lifestyle modifications like mindfulness, sleep, and visceral manipulation may reduce IBS symptoms.
Remember, what you eat is important for health and disease prevention.
What you absorb (breaking down the food) and assimilate (gets into the cells) is critical.
Test don’t guess.
Contact me to schedule an appointment to review your personalized nutritional health.
© Amy Archer RDN, CLT, CHWC